Mamae ā-waewae me rekereke Heel and foot pain (plantar fasciitis)
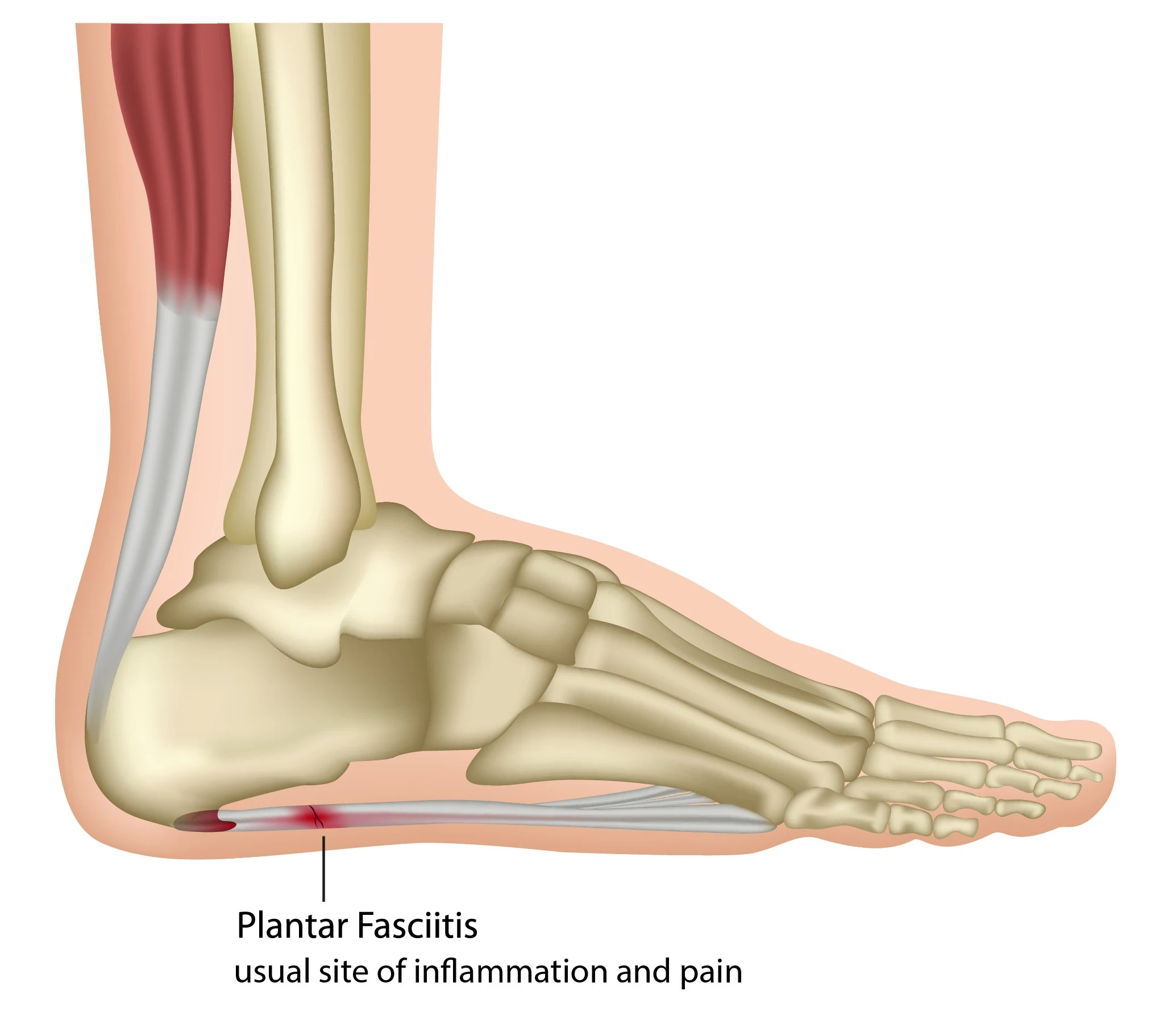
Plantar fasciitis is a common cause of pain under one of your heels. The plantar fascia is a strong flat band of connective tissue (like a ligament). It acts like a bow string and supports the arch of your foot by connecting your heel bone to the bones in the front of your foot.
Causes of plantar fasciitis
Plantar fasciitis is inflammation and pain in your plantar fascia. It affects around 1 in 10 people and is more common in women than men. You are more likely to get plantar fasciitis if you:
- are on your feet a lot for work (for example, nurses and retail staff)
- do a lot of walking, running or standing when you are not used to it
- wear unsupportive footwear with poor cushioning for walking, running or standing
- are overweight (this puts strain through the arch of your foot)
- quickly increase how much or how intensely you exercise, leading to overuse
- have a tight Achilles tendon.
Symptoms of plantar fasciitis
When the arch of your foot is under more stress, it can cause tiny tears in your plantar fascia, usually where it connects to your heel bone. This causes inflammation and pain under or around your heel when standing or walking. It might even be painful while resting.
Other symptoms include:
- 'first-step pain' (after getting out of bed or sitting) — a feeling on your heel or under your foot like stepping on a stone
- pain after driving
- deep aching in your foot
- pain that is worse when you are barefoot or walking up stairs.
Diagnosing plantar fasciitis
Your healthcare provider, podiatrist or physiotherapist can usually diagnose plantar fasciitis by talking to you and examining your foot. You might have an x-ray or ultrasound scan if they are not sure of the diagnosis.
Self care to reduce heel and foot pain
Plantar fasciitis usually gets better by itself, but it can sometimes take years. To help make yourself more comfortable, reduce pain and speed up your recovery:
- wear appropriate supportive shoes
- do not overtrain for sports
- warm up and cool down with activity
- do flexibility exercises — the long calf stretch, short calf stretch and static isotonic hold can help with heel pain
- if you are overweight, try losing some weight
- ice to the painful area for 20 minutes a day — put the ice in a bag or a cloth, not directly against your skin — but if you have peripheral neuropathy or nerve damage, do not use ice on your feet
- avoid walking or running on hard surfaces, particularly in bare feet
- massage your plantar fascia from the ball of your foot back to your heel — roll your foot over a tennis ball or something similar on the floor.
Treating plantar fasciitis
Ask your healthcare provider whether taking an anti-inflammatory medicine (an NSAID) would be suitable for you. NSAIDs can have some serious side effects, especially if you take them for a long time, including:
- stomach pain
- bleeding from a stomach ulcer.
If you have asthma, high blood pressure, kidney failure or heart failure you might not be able to take NSAIDs, even for a short time. If you are not sure if you can take NSAIDs, check with your healthcare provider or pharmacist.
Getting help for plantar fasciitis
If you have tried these steps and your pain is no better, you may need to see a podiatrist or physiotherapist to help with treatment.
Allied health (podiatry) — Healthpoint (external link)
Find a podiatrist — Podiatry NZ (external link)
Allied health (physiotherapy) — Healthpoint (external link)
Find a physio — Physiotherapy New Zealand (external link)
Podiatrists
A podiatrist can look at what is causing your pain and make sure the way you walk is not causing more foot problems. They may also suggest:
- strapping for your feet
- special insoles called orthotics
- wearing different shoes
- doing some stretches
- further tests or assessments.
You will usually have to pay privately to see a podiatrist. ACC may cover treatment for pain caused by an injury.
Physiotherapists
A physiotherapist can help with massage and joint mobilisation. They can suggest ways to decrease the load you put on your foot.
You may get exercises to strengthen your foot, ease your pain and help to prevent future pain.